Sex Difference in the Effect of Body Mass Index and Stress on High-Risk Diabetes Mellitus in Korean Adults
한국 성인의 고 위험 당뇨에 대한 스트레스와 체질량 지수의 성별 차이
Article information
Abstract
Purpose: This study aimed to investigate sex differences in the effect of body mass index (BMI) and stress on high-risk diabetes mellitus (DM). Methods: Secondary analysis of data from 4,271 male and female adults participating in the Sixth Korea National Health and Nutrition Examination Survey 2015 was performed. The participants were evaluated using questionnaires and blood tests. Data were analyzed using descriptive statistics, t-test, χ2-test, and multiple logistic regression analysis (SPSS 24.0). Results: To identify sexspecific effects, interaction variables were included. Hemoglobin A1c (HbA1c) level was higher in men than in women, and the risk of DM decreased 0.31 times in women compared to that in men. As age increased, the odds of risk DM increased 1.03. The risk of DM increased 1.99 times in overweight individuals and 2.79 times for obese individuals compared to that in individuals with normal weight. Stress levels were higher in women than in men, but stress is not an influential factor in high-risk DM. In age-sex interaction, the odds of risk DM increased 1.02 in women compared to that in men as age increased. Conclusion: HbA1c level was affected by age-sex interaction, and age and sex should be considered in the application of HbA1c in the diagnosis of DM.
Introduction
Globally, 382 million individuals are estimated to have diabetes, and type 2 diabetes mellitus (DM) is expected to affect nearly 10% of the world’s population by 2035 [1]. More than 25% of the US population aged 65 years has DM [2]. Aging of the overall population is a significant driver of the DM epidemic, and DM in older adults is linked to higher mortality, reduced functional status, and increased risk of institutionalization [3].
The epidemic of type 2 DM is clearly linked to increasing overweight and obesity rates in the US population [4]. Obesity is a condition in which fat tissue excessively accumulates in the body and causes chronic diseases such as type 2 DM, hypertension, dyslipidemia, and cardiovascular disease [5,6]. The association between visceral obesity and risk of type 2 DM differs by sex, age, and race, and various anthropometric indicators remain poorly understood [6]. It has been established that subjects with increased body mass index (BMI) are susceptible to type 2 DM [7]. Several factors contribute to DM pathogenesis, including psychological factors [8]. Moreover, the prevalence of DM substantially increased because of the epidemic of obesity [7].
Previous studies have reported that patients with DM are at least twice at risk of having depression, anxiety, and stress compared to the general population [9]. Stress level was higher in women than in men based on the hormone difference due to sex and difference in specific brain activation that recognizes emotion [10]. DM and stress are significantly associated with Hemoglobin A1c (HbA1c) [8]. Severe stressors were associated with poorer glycemic control [11]. This chronic stress affects obesity indicators such as body fat mass and abdominal obesity [12]. Furthermore, the clinical DM evaluation reported that the level of DM-related psychological distress among patients with DM is >30% [13].
The data from previous studies have suggested that HbA1c helps in detecting undiagnosed DM, especially in high-risk subjects [14]. HbA1c is a form of hemoglobin that is measured to identify the average concentration of plasma glucose over the relatively long period of 2–3 months prior to the date of measurement [15]. In 2011, the World Health Organization (WHO) and American Diabetes Association accepted the HbA1c level ≥6.5% as a diagnostic criterion for DM and HbA1c level of 5.7%–6.4% for high-risk DM [16].
An obesity-related advanced study based on the national health nutrition survey in our country examines mostly the change and trend in the obesity rate based on BMI [17]. Women had significantly lower BMI, more support and confidence in living with DM (22% of the variance) [18], and men have worse control conditions of blood lipid levels [19], so it is necessary to confirm according to sex.
Previous studies have included obesity and DM [6,7,14], stress, and DM in the evaluation [8,9,11,13]. However, there are limited studies on DM that combine physical factors such as obesity and emotional stress. Particularly, there are few studies on the effect of obesity and stress on high-risk DM in Korean adults based on sex. Moreover, the Sixth Korea National Health and Nutrition Examination Survey 2015 (KNHANES VI-3) collected representative, nationwide data and therefore presented a suitable sample to establish reference values in Korea adults. Thus, in this study, we attempted to identify sex differences in the effects of BMI and stress on high-risk DM (HbA1c level, 5.7%–6.4%). We would like to provide basic data on the prevention of DM.
Methods
1. Research design
This study is a descriptive survey study that includes a secondary analysis of KNHANES VI-3 raw data to investigate potential changes in HbA1c levels in BMI and stress in South Korean adults based on sex.
2. Samples and setting
Data of adult participants (>19 years of age) were extracted from KNHANES Ⅵ-3 conducted by the Ministry of Health and Welfare and the Korea Centers for Disease Control and Prevention, and those who were diagnosed with DM with missing data were excluded.
The 4,271 included participants were divided into groups based on sex: male (n=1840, 43.1%) and female participants (n=2431, 56.9%).
3. Analyzed parameters
In this study, general participant characteristics consisted of age, sex, education level, height, and weight.
1) BMI
Height and weight were measured after an overnight fast with participants wearing light clothing. According to the definition of the WHO, a BMI >25 kg/m2 is classified as overweight and that >30 kg/m2 as obesity [5]. Nevertheless, this classification is not appropriate for Asian individuals as it was developed based on data obtained for the Western population [20]. Instead, the BMI classification of the WHO Western Pacific regional office was employed in this study [21], which defines a BMI of <23 kg/m2 as normal weight, 23–24.9 kg/m2 as overweight, and ≥25 kg/m2 as obesity.
2) Stress
Stress level was classified based on the answers for the question “How much stress do you feel in ordinary days?” The choices include “does not feel much,” “feel a little,” “feel much,” and “feeling very much,”
3) Blood parameters
Blood samples were collected in the morning following an overnight fast (≥8 h), and blood was drawn from the median cubital vein using a vacutainer needle and collected in a vacuum tube. HbA1c level was measured using high-performance liquid chromatography (HLC-723G7, Tosoh, Japan).
The high-risk DM group (HbA1c level, 5.7–6.4%) and normal group (HbA1c level <5.7%) were classified by HbA1c level [14]. In this study, 30.9% of the participants are assigned to the high-risk DM group and 69.1% in the normal group.
4. Ethical considerations
KNHANES VI-3 was reviewed by the Korea Centers for Disease Control and Prevention Institutional Review Boards (approval number of 117002). Anonymity and confidentiality of the participants were guaranteed by coding personal information with assigned serial numbers. According to the raw data sharing regulation of the Korea Centers for Disease Control and Prevention, data from the national survey were provided after we were granted permission to use the data (June 3, 2018) and we subsequently initiated our assessments.
5. Data analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS, version 24.0, Chicago, IL, USA). General participant characteristics were analyzed with descriptive statistics. Differences in BMI and stress relative to sex were analyzed using t-test and χ2-test. The predictive variables for high-risk DM were determined by multiple logistic regression analysis. We obtained 2-tailed signicance levels for all statistical tests, and a P-value <0.05 was considered statistically significant.
Results
1. Sex differences in general characteristics
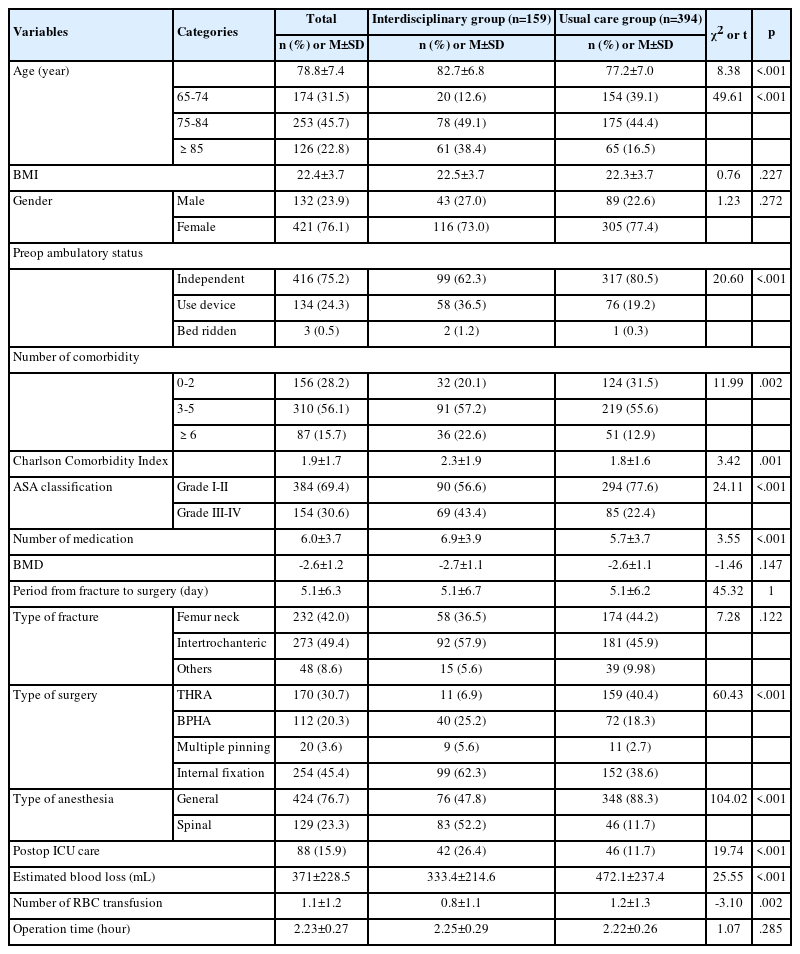
The average age of the participants was 49.6 years. The HbA1c level was higher in men than women (t=2.80, p=.005). The high-risk DM group included more men (32.4%) than women (29.7%) (χ2=3.38, p=.031) (Table 1).
2. Sex differences in BMI and stress
In BMI, 27.2% and 38.4% of men were overweight and obese, respectively. Moreover, 21.2% and 29.7% of women were overweight and obese, respectively. The prevalence of overweight and obesity was higher in men than in women (χ2=93.14, p<.001). The stress level was higher in women than in men (χ2=18.21, p<.001) (Table 2).
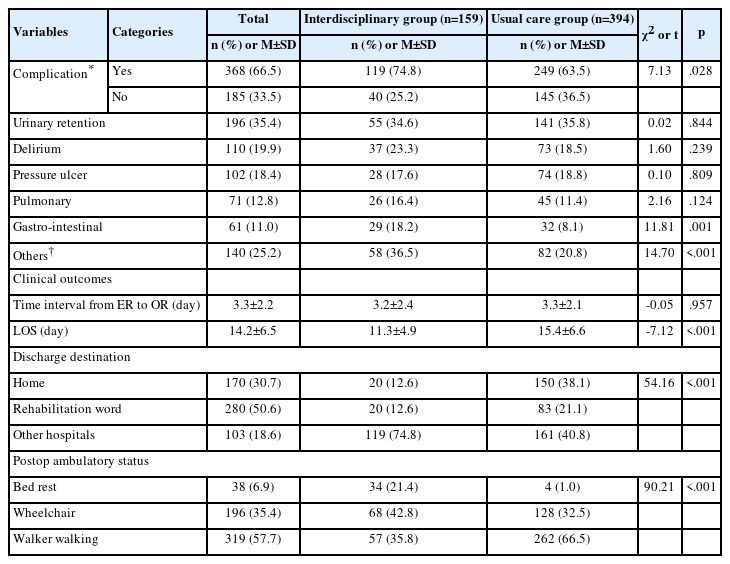
3. Factors affecting high-risk DM
In Model I, multiple logistic regression analysis including sex, age, BMI, and stress were performed to identify the influencing factors of high-risk DM. As a result, age and BMI were influential factors. Specifically, as the age increased, the odds of risk DM increased 1.06 (95% CI, 1.05–1.06; p<.001). In BMI, the risk of DM increased 1.82 times (95% CI, 1.51–2.19; p<.001) in overweight individuals and 2.58 times (95% CI, 2.18–3.06; p<.001) in obese individuals compared to that in individuals with normal weight. Stress and sex were not influential factors of high-risk DM.
In Model II, in order to identify sex-specific effects, the study focused on age and BMI, which are influential factors of high-risk DM in Model I. Interaction variables (age-sex and BMI-sex) were included in the multiple logistic regression analysis. As a result, sex, age, BMI, and age-sex were considered influential factors. Specifically, based on sex, the risk of DM decreased 0.31 times (95% CI, 0.12–0.76; p=.001) in women compared to that in men. As the age increased, the odds of risk DM increased 1.03 (95% CI, 1.01–1.05; p=.001). In BMI, the risk of DM increased 1.99 times (95% CI, 1.52–2.60; p<.001) in overweight individuals and 2.79 times (95% CI, 1.67–4.65; p<.001) in obese individuals compared to that in individuals with normal weight.
In the age-sex interaction, the odds of risk DM increased 1.02 (95% CI, 1.01–1.03; p=.001) in women compared to that in men as age increased. There was no significant difference in the BMI-sex interaction. In other words, as BMI increased, there was no difference in the effect on high-risk DM based on sex (Table 3).
Discussion
This study aimed to identify sex differences in the effect of BMI and stress on high-risk DM in Korean adults. To identify sex-specific effects, interaction variables were included in the analysis. As a result, sex, age, BMI, and age-sex interaction were influential factors of high-risk DM.
In this study, HbA1c level was higher in men than in women, and there were more men (32.4%) than women (29.7%) in the high-risk DM group. The risk of DM decreased 0.31 times in women compared to that in men. HbA1c levels in men were higher than those in women [15]. Furthermore, in different sex groups, HbA1c levels gradually increase with increasing age [22]. It is most likely because factors such as blood pressure in adult men had worse control conditions and women may be easily affected by the physiological cycle [18]. It is possible that this finding is related to lower hemoglobin levels in menstruating women with more rapid erythrocyte turnover, as suggested previously [19].
In this study, as age increased, the odds of risk DM increased 1.03. The HbA1c level is higher in individuals aged ≥60 years than in those aged <30 years [23]. HbA1c levels were positively correlated with age in Chinese [15], and Japanese adults [24]. As the age increased, the HbA1c level increased to 5.7%–6.4% compared to the baseline level of 5.6% [25]. This indicated that age is a significant independent influential factor of HbA1c. It seemed that blood glucose level increases with age incrementally so that HbA1c levels also increased, especially with advancing age. Moreover, HbA1c is a form of hemoglobin, which may affect the hemoglobin level in women due to their physiology, so it seems to be different according to sex.
In this study, BMI is higher in men than in women, and the risk of DM increased 1.99 times in overweight individuals and 2.79 times in obese individuals compared to that in individuals with normal weight. Based on the BMI, the HbA1c level was 5.7%–6.4% higher than that of 5.6% [25]. Increased BMI among adults with DM reflected better HbA1c level [18]. In both men and women, the group with increased HbA1c level showed obesity. Particularly, there was a difference between the HbA1c group with level <6.0% and those with level >6.1%. A positive correlation between BMI and HbA1c was reported. Moreover, BMI was an influential factor of HbA1c [26]. Obesity (26.4%) among adults with DM led to poorly controlled HbA1c levels (67%) [27]. The risk of developing metabolic syndrome according to the HbA1c level increased more rapidly with the higher HbA1c level in women than in men [26]. These results are associated with increased blood glucose levels in obese individuals, and the increase in HbA1c level was due to increased body weight.
In this study, stress levels were higher in women than in men, and stress is not influential factor of high-risk DM. Stress symptoms have been positively linked with DM, and women were found to be at risk of stress in the study [9]. Stress was the major significant contributor when it was mild or moderate. The HbA1c level was 1.47 times and 1.68 times for severe stress levels [28]. This study result was in contrast to the results of general studies because it had limited appropriate stress evaluation by investigating stress level only through one question. Therefore, future research should involve stress measurement tools and cortisol as a stress hormone.
Stress symptoms strongly affect glycemic HbA1c control. In fact, those psychiatric symptoms remained as important independent risk factors for DM [28]. It seemed that stress affects obesity indicators such as BMI and increases the risk of obesity. Moreover, obesity is an influential factor of DM, so the risk of DM increases with increasing stress.
In this study, in the age-sex interaction, the odds of risk DM increased 1.02 in women compared to that in men as age increased. Sex differences were noted in the relationship between HbA1c level and age [22]. The analysis of the HbA1c levels gradually increased with age until 79 years [15]. Tissue sensitivity to insulin decreases as age increases, and HbA1c level is particularly increased in menopausal women than in men. In other words, as the age and sex interact, the blood glucose and HbA1c levels increase, especially with age [29]. Age and sex should be considered in the application of HbA1c in the diagnosis of DM and are intended to provide basic data for prevention and management of DM in Korean adults.
Conclusion
To identify sex-specific effects, interaction variables were included in the study. Sex, age, BMI, and age-sex interaction were influential factors of high-risk DM. In sex, the risk of DM decreased in women compared to that in men. As age and BMI increased, the risk of DM increased. In the age-sex interaction, the risk of DM increased in women compared to that in men as age increased.
It is meaningful that the study clearly demonstrates that age-sex interaction affects HbA1c levels in South Korean adults, indicating that HbA1c levels differ by age and sex and contributes to the prevention of DM. Moreover, this can be used as fundamental data to establish a DM nursing program for Korean adults.
CONFLICT OF INTEREST
The authors declared no conflict of interest.